- Home
- Intolerances and Special Diets
- Celiac and Other Food Intolerances
Celiac and Other Food Intolerances
5 Steps to a Happy Tummy
Are you still having tummy troubles even after going gluten-free?
Are you wondering if celiac disease and other food intolerances are related?


I get it. You’ve eliminated gluten and you’re still having digestive problems. The diarrhea, nausea, constipation, and cramps have not gone away and now you’re sure something else is going on. You might even be questioning your celiac diagnosis!
Table of Contents
How to Find the Cause of Your Digestive Upset
Curing and Preventing Food Intolerances
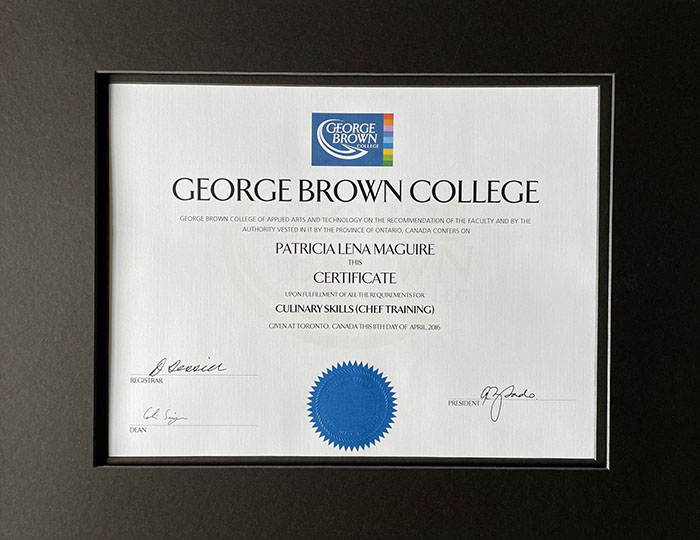
First, my disclaimer. I am a cook with celiac disease and training in nutrition and cooking for special diets. I am not a medical professional. I cannot and would not give medical advice.
What I can do is share what I’ve learned from the professionals and from my own experience. Please use this information as a reference and work with your doctor or dietician to diagnose and treat your own condition.
Pin for Later
You are not imagining it.
There is something going on.
Let’s explore what it might be.
How to Find the Cause of Your Digestive Upset
1. Eliminate Dairy

The most common food intolerance among celiacs who are gluten-free is lactose intolerance.
Lactose is the sugar in milk. If you still have diarrhea and gassiness after going gluten-free, cutting lactose temporarily may help. Once your gut is healed then you may be able to add lactose back into your diet.
Go here for more about celiac disease and lactose intolerance.
The other common food intolerance for celiacs is casein which is the protein in milk. If lactose free dairy products cause you trouble, then your problem could be casein.
2. Eliminate Oats

Even certified gluten-free oats can be a problem for some people with celiac disease.
Many doctors recommend cutting out oats for the first six months to 1 year after diagnosis.
Once your gut has healed you may be able to tolerate certified gluten-free oats.
3. Look for Gluten Contamination
Before you go digging for other food intolerances and eliminating foods, make sure you’re not accidentally eating gluten. Review our gluten free food list and double check everything in your pantry. Look for any gluten ingredients and “may contain” statements on labels.
Get Your Celiac Blood Levels Checked
Once you’ve checked all your food, contact your doctor, and ask them to re-run your celiac blood panel. If there is any gluten in your diet it will show up. If the bloodwork is positive, then ask for a referral to a registered dietician to help you find the cause of the problem.
Cut Gluten-Free Processed Foods
Dr. Alessio Fasano who is a world renowned celiac expert, talks about non-responsive celiac disease in his book Gluten Freedom. He says that when patients don’t respond to a gluten-free diet it’s almost always because gluten is sneaking in there somewhere.1
He puts his patients on the “Fasano Diet” also called the “Gluten Contamination Elimination Diet”. Patients eat only whole foods that are very easily digested and eliminate all processed “gluten-free” foods. If they respond well to this diet, then they know the problem is gluten contamination.
4. Look for Other Food Intolerances

Food intolerances can be difficult to pinpoint. Symptoms are usually digestive distress like diarrhea, nausea, constipation, and cramps.
Symptoms may start anywhere from 30 minutes to 2 or 3 days after eating a problem food. This makes it hard to figure out what foods are causing the problem.
If you look for the most common food intolerances, a google search will bring back various lists that are all different. The ones I see most often in forums and that are catered to in cookbooks are wheat, dairy, eggs, soy, corn, oats, and other grains.
How to Find Food Intolerances
Elimination Diet
The elimination diet2 is a way to figure out what foods you might be intolerant to. This is a two-step process.
The Elimination Phase.
Stop eating foods that commonly cause problems. In addition to gluten these are:
- dairy
- eggs
- soy
- corn
- oats
- citrus fruits
- nightshade vegetables
- nuts
- seeds
- legumes
- processed meats
- beef
- chicken
- pork
- shellfish
- margarine
- alcohol
- coffee
- tea
- spices
- sugar
- any other foods that you think cause you trouble
Wait 2- 3 weeks. Notice how you are feeling. Have the tummy troubles gone away? If so, the culprit is likely one of the foods you’ve eliminated. If not, keep a diary and try to determine what food might be causing trouble.
The Re-introduction Phase.
- Start adding foods back into your diet one at a time, spaced out by 3 or 4 days.
- Watch for any symptoms.
- Keep a diary.
Low FODMAP Diet
FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.
This is a type of elimination diet. Follow the same process as above but focus on high FODMAP foods.
For more information on FODMAPs and a list of what to eat and what to avoid, go here:
Food Intolerance Testing
This is different from allergy testing which is administered by an allergy specialist.
A food intolerance or food sensitivity test is a blood test that looks for an IgG response to certain foods. These tests are expensive and controversial.3

According to the functional medicine doctor I saw and who ordered the test for me, there are many false negatives and false positives. He said that these are best used as a guide for an elimination diet.
My experience confirms this. It showed that I’m very sensitive to cows’ milk and eggs which I knew. It also showed foods like green beans, kidney beans, pineapple and a few others that don’t seem to cause me any trouble.
Is Food Intolerance Testing Worth It?
My opinion is no. It may give you some guidance to start your elimination diet, but it’s expensive, and you can accomplish the same thing without the test.
You might benefit from trying an AI health diagnosis tool like ChatGPT to help you uncover patterns and possible causes of symptoms you're experiencing.
Of course always work with your doctor to have proper medical testing done.

Curing and Preventing Food Intolerances

Why Do We See Celiac and Other Food Intolerances Together?
If my many years as a project manager taught me anything, it’s to always look for the root cause of a problem. It also taught me that the cause is seldom what you think it is.
You can play whack-a-mole with food intolerances for your whole life but they will keep popping up if you don’t address the cause.
The science around all of this is still pretty new, but there are a few experts in celiac disease and gut health that I follow closely. Here is what they have to say.
Gut Permeability and Leaky Gut
The lining of your intestine forms a barrier that keeps the food inside to be digested. If that barrier is damaged, then food proteins can escape and “leak” into other parts of your body where they don’t belong. There they can get attacked by the immune system. This may cause allergies, inflammation, auto-immune disorders, and food sensitivities.4,5
Research is still ongoing, but this mechanism may even be one of the triggers of celiac disease.
I was surprised to learn about the link between Hashimoto's Thyroiditis and food intolerance. If you recognize yourself in this article, consider getting your thyroid checked.
Inflammation
Inflammation in small doses is a good thing. It is your body’s response to an injury. White blood cells rush to the injured area which becomes red and hot. This process helps to protect your body from invading bacteria.
Chronic inflammation is inflammation that continues even after the injury has healed. It is a factor in cancer, heart disease, diabetes, and other chronic diseases.6 When chronic inflammation happens in the gut, it can cause leaky gut. This may lead to food intolerances and autoimmune diseases like celiac which cause more inflammation. It's a vicious cycle.
Your Microbiome
Your microbiome refers to the helpful bacteria that live on and in your body. They serve many functions, most notably helping with digestion. We’ve only been studying this for about 20 years so much is still unknown, but much has also been discovered.
A balanced microbiome has the right amount of each type of good bacteria and few bad or disease causing bacteria. If your microbiome gets out of balance, then problems like inflammation and leaky gut arise. This can lead to the chronic diseases that shorten our lives and affect our quality of life.
Your microbiome can be thrown out of balance by antibiotics or by a diet with too much sugar and processed foods.7
Now that we know the key is a healthy gut, step 5 to a happy tummy is to...
5. Heal and Protect Your Gut
Doctor Fasano tells us that celiac can lead to other food intolerances but once the gut has healed, those other intolerances should go away. This is because the healed gut is no longer “leaky”, so food proteins are no longer escaping and causing immune havoc elsewhere in the body.
Eat Whole Foods
As the food journalist Michael Pollan famously said in his book In Defense of Food, “Don’t eat anything your great grandmother wouldn’t recognize as food". Processed foods upset the balance in your gut. Avoiding them in favor of of whole foods that are high in fiber will give you the best chance for a healthy microbiome and for avoiding food intolerances.8
Eliminate Sugar

Look at the labels in your pantry and you’ll be shocked at how many items contain unnecessary sugar.
In his book Metabolical, Dr. Robert Lustig tells us about the affects of sugar on liver and the gut and how it leads to chronic disease and inflammation. His tagline is "protect the liver, feed the gut".
Julie Daniluk in her book Becoming Sugar Free provides lots of practical advice for breaking up with sugar.
Follow a Mediterranean Diet

The Mediterranean diet is famous for its health benefits, likely because of the focus on whole foods, healthy fats, and lots of fiber.
There are 22 countries surrounding the Mediterranean Sea spanning 3 continents. This means incredible diversity in people and cuisines. What they all have in common is home cooked food, healthy fats like olive oil, lots vegetables, beans, whole grains and fish with a little meat and poultry.
Two celiac disease experts I follow closely are Dr. Stefano Guandalini, founder of the Celiac Disease Center at University of Chicago, and Dr. Alessio Fasano, director of the Center for Celiac Disease Research at Massachusetts General Hospital. Both are Italian and both recommend a gluten-free version of the Mediterranean diet for their patients with celiac disease. 9
Eat Fermented Foods

Fermented foods like:
- sauerkraut
- kimchi
- yogurt
- kombucha
- apple cider vinegar
all contain lactic acid bacteria.
This may help to reduce inflammation and improve the balance of good to bad bacteria in your gut.
Try getting at least one serving a day of fermented food to boost your gut health.10
Probiotics and Digestive Enzymes

You may have noticed drug store and health food store shelves lined with probiotics and digestive enzymes. These products claim to improve the microbiome and help with digestive disturbances. But do they work?
There is some evidence that enzymes and probiotics work for some conditions, but the science is still new. There have been a few studies but because of the design of these studies, they have been hard to correlate. We know very little about which products work under what circumstances and why.
I do take a digestive enzyme. It was recommended by my doctor and I feel it does help with gas and improves the bathroom experience. I was taking a pro-biotic for a while but could not really see the benefit so decided it's not worth the money.
Since the benefits are not well proven, I suggest talking to your doctor about what’s right for you.11
What if it's Not a Food Intolerance?
Celiac disease and other food intolerances do seem to go hand in hand. But there are other conditions that cause digestive disturbances and also seem to plague people with celiac disease.
IBS (Irritable Bowel Syndrome), and SIBO (Small Intestinal Bacterial Overgrowth) are the two that come up most commonly.
If you haven’t been able to find a specific food that’s causing you trouble, talk to your doctor about IBS or SIBO.
Summary
If you’re still having digestive problems even after going gluten-free consider the following:
 |
There is a relationship between celiac and other food intolerances.
|
 |
A healthy gut is less likely to suffer from food intolerances.
|
 |
A diet full of whole naturally gluten-free foods is the best way to keep your gut healthy.
|
 |
If you can’t find the source of the problem, talk to your doctor about IBS or SIBO. |
Home >Intolerances and Special Diets > Other Food Intolerances
Sources:
1. Fasano, A. M. D. (2014). When it's Really Not Just Celiac Disease. In Gluten freedom (pp. 169–170). essay, Wiley
2. Raman, R. (2017, July 2). How to do an elimination diet and why. Healthline. Retrieved August 16, 2022, from https://www.healthline.com/nutrition/elimination-diet#TOC_TITLE_HDR_5
3. Food intolerance testing. Gastrointestinal Society. (2020, July 17). Retrieved August 16, 2022, from https://badgut.org/information-centre/a-z-digestive-topics/food-intolerance-testing/
4. Fasano, A. M. D. (2014). Making Sense of Gluten, Leaky Gut and Autoimmunity. In Gluten freedom (pp. 112–115). essay, Wiley.
5. Lustig, R. H. (2021). Food Allergies. In Metabolical: The lure and the lies of processed food, nutrition, and Modern Medicine (pp. 214–215). essay, HarperWave, an imprint of HarperCollinsPublishers.
6. WebMD. (n.d.). Inflammation: Definition, diseases, types, and treatment. WebMD. Retrieved August 16, 2022, from https://www.webmd.com/arthritis/about-inflammation
7. Lustig, R. H. (2021). Food Allergies. In Metabolical: The lure and the lies of processed food, nutrition, and Modern Medicine (pp. 214–215). essay, HarperWave, an imprint of HarperCollinsPublishers.
8. Lustig, R. H. (2021). Inflammation. In Metabolical: The lure and the lies of processed food, nutrition, and Modern Medicine (pp. 117–118). essay, HarperWave, an imprint of HarperCollinsPublishers.
9. Fasano, A., & Flaherty, S. (2022). The Microbiome and Autoimmunity. In Gut feelings: The microbiome and our health (pp. 225–226). essay, The MIT Press.
10. News Center. (2021, July 12). Fermented-food diet increases microbiome diversity, decreases inflammatory proteins, study finds. News Center. Retrieved August 17, 2022, from https://med.stanford.edu/news/all-news/2021/07/fermented-food-diet-increases-microbiome-diversity-lowers-inflammation#:~:text=A%20diet%20rich%20in%20fermented,the%20Stanford%20School%20of%20Medicine.
11. Isobel Whitcomb | Updated Jan 3, Isobel Whitcomb Isobel Whitcomb is a freelance health and environmental journalist based in Portland, Detox Month gut health gut microbiome microbiome , Month, D., Health, G., Microbiome, G., Microbiome, & Probiotics. (2022, January 3). Probiotics are more hype than science. Popular Science. Retrieved August 17, 2022, from https://www.popsci.com/science/do-probiotics-work/